What Is Interoperability in Healthcare? - A Comprehensive Guide
Summarize this article with:
✨ AI Generated Summary
Healthcare data interoperability enables seamless exchange and use of patient information across diverse systems, improving care quality, reducing errors, and lowering costs. Key standards like HL7 FHIR, CDA, and SNOMED CT support structured, semantic data exchange, while technologies such as federated learning and homomorphic encryption enhance privacy-preserving analytics and AI collaboration. Implementation challenges include legacy system integration, security requirements, and regulatory compliance, with tools like APIs, HIEs, cloud platforms, blockchain, and Airbyte facilitating effective interoperability solutions.
Healthcare providers frequently struggle to access complete patient information across different systems, leading to care gaps and inefficient treatment decisions.
Healthcare data interoperability solves this fundamental challenge by enabling seamless data exchange between disparate healthcare systems, applications, and devices.
This comprehensive guide explores the current landscape of healthcare interoperability, emerging technologies, and practical implementation strategies that healthcare organizations can leverage to improve patient outcomes while maintaining data security and regulatory compliance.
What Is Healthcare Data Interoperability and Why Does It Matter?
Healthcare data interoperability represents the ability of different healthcare applications, devices, and systems to exchange, access, integrate, and use data in a coordinated manner. This capability extends within and across organizational, regional, and national boundaries, allowing healthcare providers to seamlessly share patient health information.
When healthcare providers can access complete and up-to-date information through interoperable systems, they optimize health outcomes for individuals and populations while reducing administrative burden and healthcare costs.
Why Is Healthcare Data Interoperability Essential for Modern Healthcare?
Data interoperability in healthcare delivers transformative benefits across multiple dimensions of healthcare delivery:
- Maximizes Operational Efficiency: Interoperability eliminates administrative burden by reducing repetitive data entry tasks and enabling healthcare practitioners to focus on direct patient care.
- Improves Patient Care Quality: When clinicians can access complete patient health information, including medical history, current medications, allergies, and recent test results, they deliver more accurate diagnoses and appropriate treatments.
- Reduces Medical Errors and Associated Costs: Medical errors cost the healthcare system billions annually, but data interoperability significantly reduces these incidents by providing physicians with comprehensive patient data and eliminating manual re-entry of existing medical information.
- Enhances Patient Engagement and Experience: Interoperable systems empower patients to take active roles in their healthcare management by providing access to their complete medical histories, test results, and educational resources.
- Reduces Healthcare Costs Across the System: Better patient care through interoperability results in reduced hospital readmissions, fewer complications, and the elimination of unnecessary procedures and tests.
What Are the Primary Challenges in Achieving Healthcare Data Interoperability?
Healthcare organizations face several critical obstacles when implementing comprehensive interoperability solutions:
- Legacy Systems Integration Complexity: Many healthcare organizations operate on outdated systems that lack modern integration capabilities, creating data silos and compatibility challenges.
- Budget and Resource Constraints: Comprehensive interoperability initiatives require significant investments in new hardware, software licenses, staff training, and system integration services.
- Data Privacy and Security Requirements: Patient health information represents highly sensitive data requiring robust security measures, including end-to-end encryption, granular access controls, and multi-factor authentication.
- Lack of Standardization and Coordination: The absence of uniform systems and standards across healthcare organizations complicates data exchange and creates interoperability gaps.
What Do Current Federal Regulations Require for Healthcare Interoperability?
The Centers for Medicare and Medicaid Services (CMS) and the Office of the National Coordinator for Health Information Technology (ONC) have implemented comprehensive federal measures to advance healthcare interoperability through mandatory standards adoption and enhanced digital capabilities.
21st Century Cures Act
The Cures Act prohibits information blocking practices that materially discourage access to Electronic Health Information (EHI), with penalties up to $1 million for non-compliance. The Act requires healthcare providers and technology developers to implement FHIR-based APIs that enable patients and authorized third parties to access health information electronically.
CMS Interoperability Final Rules
The CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) streamlines prior authorization processes while ensuring patients remain central to authorization decisions. The CMS Interoperability and Patient Access Final Rule (CMS-9115-F) mandates that patients can access and use their health data through third-party applications of their choice, promoting patient-controlled data sharing.
TEFCA
The Trusted Exchange Framework and Common Agreement (TEFCA) enables secure, standardized health information exchange across networks nationwide. TEFCA priorities for 2025 include enhancing transparency through the QHIN Technical Framework updates, expanding use cases beyond treatment to include payment and public health applications, and implementing FHIR-based query capabilities for improved data access.
HTI Rules
The Health Technology and Interoperability (HTI) rules define permissible exceptions to information sharing requirements while maintaining patient access rights. These updates align with TEFCA requirements and establish clear guidelines for healthcare organizations regarding data sharing obligations and compliance requirements.
What Standards Enable Effective Healthcare Data Interoperability?
Healthcare data exists in scattered, unstructured, and inconsistent formats across different systems, making standardization essential for meaningful information exchange. Organizations must implement established protocols and standards to achieve true interoperability capabilities:
HL7 FHIR (Fast Healthcare Interoperability Resources)
FHIR represents the current standard for healthcare data exchange, utilizing RESTful web services and modern web technologies to simplify data integration processes. Released as an evolution of HL7 v2, FHIR organizes healthcare data into modular "resources" including patients, medications, observations, and care plans that integrate seamlessly with existing systems, mobile applications, and wearable devices.
HL7 Version 2
HL7 v2 continues to serve as a foundational messaging standard for healthcare information exchange, particularly in hospital systems and laboratory interfaces. While FHIR represents the modern approach to interoperability, many healthcare organizations maintain HL7 v2 implementations for specific workflows and legacy system integration.
Clinical Document Architecture
The Clinical Document Architecture (CDA) provides structured templates for clinical documents, including discharge summaries, consultation notes, and care plans. CDA documents maintain clinical context and support comprehensive documentation requirements while enabling semantic interoperability across different healthcare information systems.
DICOM and Medical Imaging Standards
Digital Imaging and Communications in Medicine (DICOM) standardizes medical imaging data exchange, enabling consistent sharing of X-rays, MRIs, CT scans, and other diagnostic images across healthcare facilities. DICOM integration with FHIR resources creates comprehensive patient records that combine structured clinical data with associated medical imaging studies.
SNOMED CT and Standardized Terminologies
SNOMED CT provides comprehensive clinical terminology that enables semantic interoperability by ensuring consistent meaning across different healthcare systems. Integration with FHIR terminology servers enables real-time access to standardized clinical concepts, supporting accurate data interpretation and clinical decision support across healthcare organizations.
How Does Healthcare Data Interoperability Function in Practice?
Healthcare data interoperability operates through systematic processes that collect, normalize, integrate, and exchange information across diverse healthcare information systems to support clinical workflows and patient care coordination.
- Data Collection and Aggregation: Healthcare organizations gather patient information from multiple sources, including electronic health records, laboratory information systems, medical devices, patient portals, and external healthcare facilities.
- Data Normalization and Standardization: Raw healthcare data undergoes transformation into consistent formats based on established standards, including HL7 FHIR, DICOM for medical imaging, and standardized terminologies like SNOMED CT and LOINC for laboratory values.
- System Integration and Data Consolidation: Normalized healthcare data from disparate systems consolidates into unified datasets that provide comprehensive patient views.
- Secure Data Exchange and Distribution: Standardized, integrated healthcare data transmits securely through FHIR-based APIs, Health Information Exchanges (HIEs), and direct system-to-system communication protocols.
- Clinical Application and Decision Support: Exchanged healthcare data supports clinical workflows, including patient monitoring, treatment planning, medication management, and population health analytics.
What Are the Four Levels of Healthcare Interoperability?
Healthcare interoperability operates across four distinct levels, each building upon the previous to create comprehensive data exchange capabilities that support clinical workflows and patient care coordination.
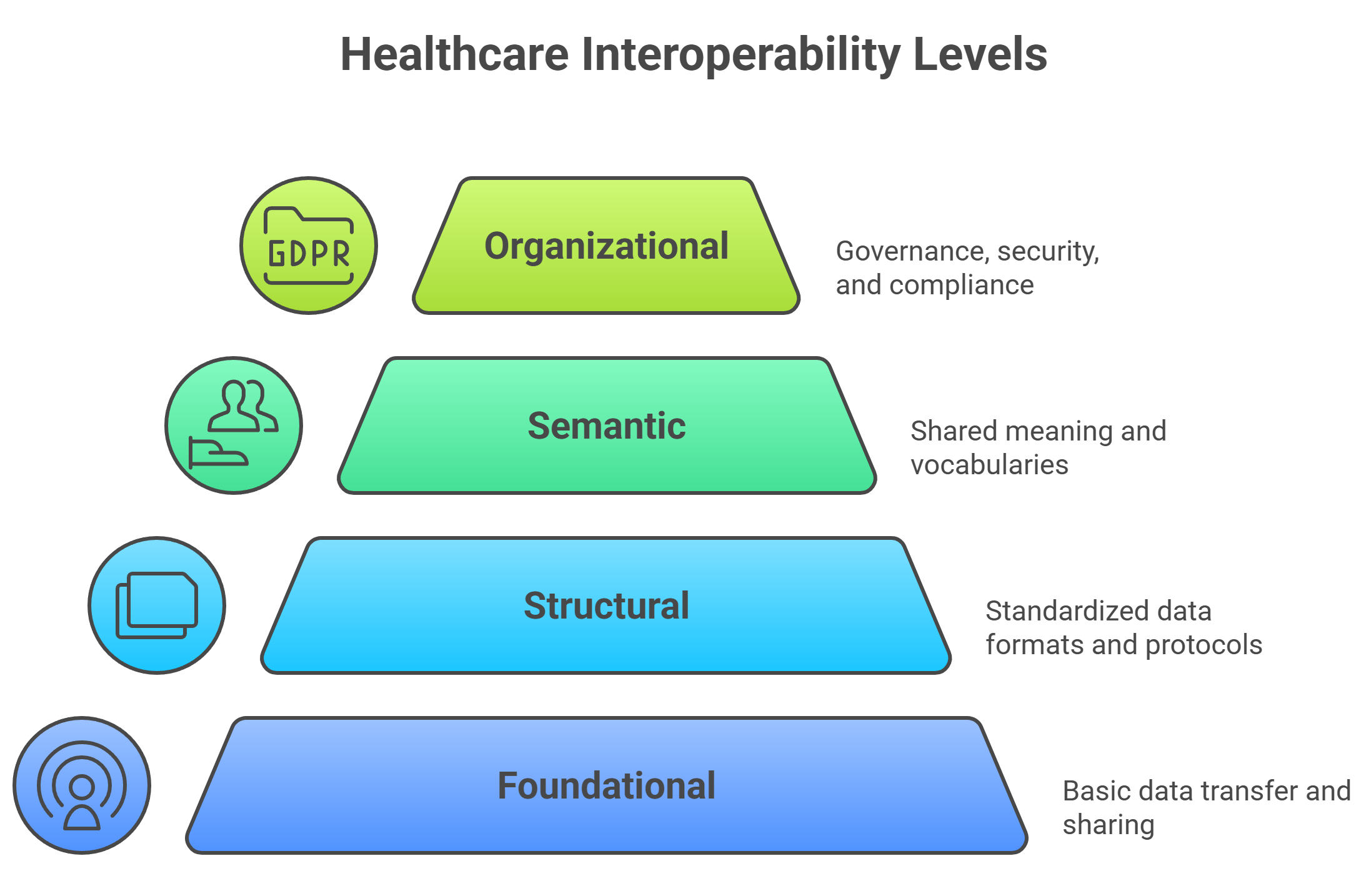
Level 1: Foundational Interoperability
Foundational interoperability enables basic data transmission between healthcare systems without requiring interpretation of the exchanged information. This level focuses on secure data transport mechanisms, including encrypted email transmission of laboratory results, file transfers between healthcare facilities, and basic electronic document sharing. While foundational interoperability ensures data reaches its destination, it does not guarantee that receiving systems can process or utilize the information effectively.
Level 2: Structural Interoperability
Structural interoperability establishes standardized data formats and syntax that enable consistent information movement between healthcare systems. Standards like HL7 FHIR and XML-based clinical documents ensure that different systems can parse and store exchanged data in appropriate database fields. This level enables automated data processing while maintaining format consistency across diverse healthcare applications and platforms.
Level 3: Semantic Interoperability
Semantic interoperability creates a shared understanding of data meaning through standardized terminologies and clinical concepts. Systems achieving semantic interoperability can accurately interpret clinical information using common vocabularies like SNOMED CT for diagnoses, LOINC for laboratory tests, and RxNorm for medications. This level enables automated clinical decision support and meaningful data analysis across different healthcare organizations.
Level 4: Organizational Interoperability
Organizational interoperability addresses governance, policy, security, and workflow alignment that enables smooth, secure, and legally compliant data exchange across healthcare organizations. This highest level encompasses privacy protections, consent management, audit logging, and regulatory compliance requirements that support comprehensive healthcare data sharing while maintaining patient trust and legal requirements.
How Can Federated Learning Transform Collaborative Healthcare AI?
Federated learning represents a revolutionary approach to healthcare artificial intelligence that enables multiple healthcare organizations to collaboratively train machine learning models without sharing sensitive patient data directly. This methodology addresses critical privacy concerns while leveraging diverse datasets to improve clinical decision support and population health analytics.
Decentralized Model Training Across Healthcare Networks
Federated learning allows hospitals, research institutions, and healthcare systems to participate in collaborative AI development while maintaining complete control over their patient data. Instead of centralizing sensitive health information, machine learning algorithms train locally at each participating site, sharing only model parameters and statistical insights. This approach enables large-scale research initiatives that would be impossible under traditional data sharing constraints.
Privacy-Preserving Clinical Research and Drug Discovery
Pharmaceutical companies and research institutions utilize federated learning to accelerate drug discovery and clinical trial optimization while maintaining patient confidentiality. This approach enables identification of potential drug candidates, biomarker discovery, and adverse event detection across multiple patient populations without creating centralized databases of sensitive health information.
Implementation Challenges and Technical Solutions
Healthcare organizations implementing federated learning must address data standardization challenges, communication latency between sites, and model bias from heterogeneous patient populations. Successful implementations require FHIR-compliant data formats, secure communication protocols, and robust governance frameworks that ensure model quality while maintaining participant autonomy.
How Does Homomorphic Encryption Enable Secure Healthcare Analytics?
Homomorphic encryption revolutionizes healthcare data analysis by enabling computational operations directly on encrypted patient data, eliminating the need for decryption during analytical processes. This breakthrough technology addresses the fundamental tension between data utility and privacy protection in healthcare analytics and research applications.
- Encrypted Data Analysis: Homomorphic encryption allows healthcare organizations to perform complex analytics, statistical analysis, and machine learning operations on encrypted patient data while maintaining complete confidentiality.
- Real-Time Clinical Decision Support: Emergency departments and critical care units can implement real-time analytics on encrypted patient monitoring data to identify deteriorating patients, predict adverse events, and optimize treatment protocols.
- Multi-Institutional Collaboration: Homomorphic encryption facilitates secure data sharing between healthcare organizations for quality improvement initiatives, clinical research, and public health surveillance without violating HIPAA privacy requirements.
What Tools and Technologies Support Healthcare Data Interoperability?
Modern healthcare interoperability relies on diverse technological solutions that address different aspects of data exchange, security, and integration across healthcare systems and organizations.
1. Application Programming Interfaces (APIs)
APIs serve as the foundation for modern healthcare data exchange, enabling secure, real-time communication between electronic health records, clinical applications, and third-party healthcare services. FHIR-based APIs provide standardized interfaces that support patient data access, clinical decision support integration, and healthcare application development while maintaining security and privacy protections.
2. Health Information Exchanges (HIEs)
HIEs create specialized networks that facilitate secure sharing of electronic health information across disparate healthcare systems, improving care coordination and reducing duplicate testing and procedures. These networks implement governance frameworks, technical standards, and security protocols that enable trusted data exchange between competing healthcare organizations while maintaining patient privacy and consent management.
3. Cloud-Based Integration Platforms
Cloud computing platforms provide scalable, cost-effective infrastructure for healthcare data storage, processing, and sharing while offering enhanced security, disaster recovery, and collaboration capabilities. Healthcare organizations leverage cloud-based solutions to modernize legacy systems, implement advanced analytics, and support remote care delivery models without significant capital investments.
4. Blockchain Technology for Data Integrity
Blockchain technology provides decentralized, tamper-resistant frameworks for healthcare data sharing that enable audit trails, consent management, and fraud prevention while maintaining data integrity across multiple participating organizations. Healthcare applications of blockchain technology include clinical trial data integrity, pharmaceutical supply chain verification, and patient consent management for research participation.
How Can Airbyte Streamline Healthcare Data Integration?
Airbyte's open-source data integration platform addresses the complex challenges of healthcare interoperability by providing enterprise-grade connectivity, security, and governance capabilities specifically designed for healthcare organizations managing sensitive patient information.
- Comprehensive Healthcare Connector Library: Airbyte's library of 600+ pre-built connectors includes specialized integrations for healthcare systems, including Epic, Cerner, FHIR APIs, laboratory information systems, and medical device platforms.
- Custom Integration Development: The platform's Connector Development Kit enables healthcare IT teams to create custom integrations for specialized medical devices, proprietary healthcare applications, and emerging health technologies.
- Healthcare-Specific Security: Airbyte implements enterprise-grade security measures specifically designed for healthcare data, including end-to-end encryption, role-based access control, and comprehensive audit logging that supports HIPAA compliance requirements.
- Real-Time Healthcare Data Synchronization: Change Data Capture (CDC) functionality ensures that critical healthcare information, including laboratory results, medication orders, and patient monitoring data, synchronizes in real-time across healthcare systems.
- Unified Clinical Data Management: The platform's support for both structured and unstructured healthcare data enables comprehensive integration of clinical notes, medical imaging metadata, and IoT device data streams into unified patient records that support holistic care coordination and clinical analytics initiatives.
- AI and Machine Learning Integration: Airbyte's vector store loading capabilities simplify the integration of healthcare data into machine learning workflows, enabling healthcare organizations to develop AI-powered clinical decision support tools, predictive analytics applications, and population health management systems.
- Advanced Analytics Implementation: Healthcare organizations can leverage Airbyte's integration with cloud analytics platforms to implement real-time patient monitoring, chronic disease management programs, and population health analytics that improve patient outcomes while reducing healthcare costs and administrative burden.
Conclusion
Healthcare data interoperability represents a critical foundation for modern healthcare delivery, enabling providers to access complete patient information while reducing errors and administrative burden. Standards like FHIR, combined with technologies such as federated learning and homomorphic encryption, provide the technical framework for secure, compliant data exchange. Organizations implementing comprehensive interoperability solutions with appropriate tools and governance frameworks can significantly improve patient outcomes while maintaining data security and regulatory compliance.
Frequently Asked Questions
What is the difference between healthcare interoperability and health information exchange?
Healthcare interoperability refers to the broader capability of different systems to exchange and use health information effectively, while health information exchange (HIE) specifically refers to the networks and infrastructure that facilitate secure sharing of electronic health information between healthcare organizations.
How does FHIR improve upon previous healthcare data standards?
FHIR utilizes modern web technologies, including RESTful APIs and JSON/XML formats, that are easier to implement and maintain compared to older standards like HL7 v2. FHIR's modular resource-based architecture enables more flexible and granular data exchange while supporting mobile applications and modern healthcare workflows.
What are the main security risks associated with healthcare data interoperability?
Primary security risks include unauthorized access to patient information, data breaches during transmission, insufficient access controls, and inadequate audit logging. Healthcare organizations must implement comprehensive security frameworks, including encryption, authentication, and monitoring, to mitigate these risks.
How long does it typically take to implement healthcare interoperability solutions?
Implementation timelines vary significantly based on organizational size, system complexity, and scope of interoperability goals. Basic FHIR API implementations may require 3-6 months, while comprehensive interoperability initiatives, including multiple systems and HIE participation, can take 12-24 months or longer.
What role do patients play in healthcare data interoperability?
Patients have increasing control over their health information through federal patient access rights that enable them to view, download, and share their health data with third-party applications and healthcare providers of their choice. Patient engagement in interoperability initiatives improves care coordination and health outcomes.

.webp)
