How Healthcare Workflow Automation Improves Patient Care?
Summarize this article with:
✨ AI Generated Summary
Healthcare workflow automation leverages AI, RPA, and intelligent systems to streamline clinical and administrative tasks, improving accuracy, reducing costs, and enhancing patient care. Key challenges include data fragmentation, cybersecurity risks, legacy system constraints, workforce shortages, and financial pressures. Advanced automation platforms enable real-time data integration, predictive analytics, and compliance monitoring, transforming operations across patient engagement, revenue cycle management, clinical decision support, and supply chain management.
- Integration of AI, ML, IoMT, and cloud-native architectures drives sophisticated, scalable automation.
- Successful implementation requires thorough needs assessment, seamless integration, robust security, and strong change management.
- Emerging technologies like generative AI, digital twins, and blockchain promise further workflow optimization and enhanced patient outcomes.
Healthcare data security breaches create significant costs while healthcare organizations simultaneously face a perfect storm of challenges with data team expansions, poor data quality issues affecting many healthcare teams, and rapidly growing healthcare data volumes.
Yet despite substantial AI implementation investments over recent years, most healthcare organizations struggle with fragmented systems that prevent them from realizing the full potential of their data investments. The healthcare workflow automation market represents both the scale of the opportunity and the urgency for data professionals to implement solutions that transform operational efficiency while maintaining the stringent security and compliance standards healthcare demands.
What Is Healthcare Workflow Automation and Why Does It Matter for Patient Care?
Healthcare workflow automation leverages advanced technologies including artificial intelligence, robotic process automation, and intelligent orchestration systems to streamline clinical and administrative processes across healthcare organizations. Manual, error-prone tasks are transformed into automated workflows that improve accuracy, reduce costs, and enable healthcare professionals to focus on high-value patient-care activities.
Modern automation extends beyond simple task replacement. Intelligent systems now adapt to changing conditions, coordinate complex multi-department processes, and provide real-time insights that support clinical decision-making. Healthcare organizations are increasingly piloting generative AI solutions as the field has evolved from basic rule-based automation to systems that understand context, make intelligent decisions, and continuously improve based on outcomes and feedback.
What Are the Current Challenges Limiting Healthcare Workflow Effectiveness?
1. Data Fragmentation and Quality Issues
Healthcare organizations typically operate multiple disparate systems including EHRs, LISs, imaging platforms, and billing systems that were not designed to work together. The resulting silos prevent comprehensive patient views and limit automation effectiveness. Poor data quality further erodes trust in automated systems across many healthcare data teams.
2. Cybersecurity and Compliance Complexity
Ransomware attacks have grown significantly over recent years, making healthcare one of the most targeted sectors. Organizations must navigate HIPAA compliance requirements and other regulations while implementing automation solutions that maintain the highest security standards as data volumes continue expanding rapidly.
3. Legacy System Integration Constraints
Outdated software often lacks modern security features and APIs, creating complex integration scenarios in environments that cannot tolerate downtime. These constraints limit the ability to implement comprehensive automation solutions.
4. Resource Allocation and Workforce Challenges
Burnout, retirements, and lack of skilled professionals create staffing shortages. Data teams work with limited resources while being tasked with increasingly sophisticated automation initiatives.
5. Financial Pressures and ROI Demonstration
Declining reimbursements and rising therapy costs force institutions to justify every technology investment with clear ROI and cost-benefit analyses. Organizations need concrete evidence that automation investments will deliver measurable improvements.
How Does Workflow Automation Transform Healthcare Operations?
Intelligent Process Orchestration
Modern platforms coordinate complex, multi-system processes across providers and payers, moving beyond simple task automation to end-to-end process optimization. These systems manage workflows that span multiple departments and external partners.
Predictive Analytics and Proactive Care Management
Machine-learning algorithms anticipate resource needs and identify bottlenecks before they occur, enabling proactive interventions that improve outcomes while reducing costs. Healthcare teams can address issues before they impact patient care.
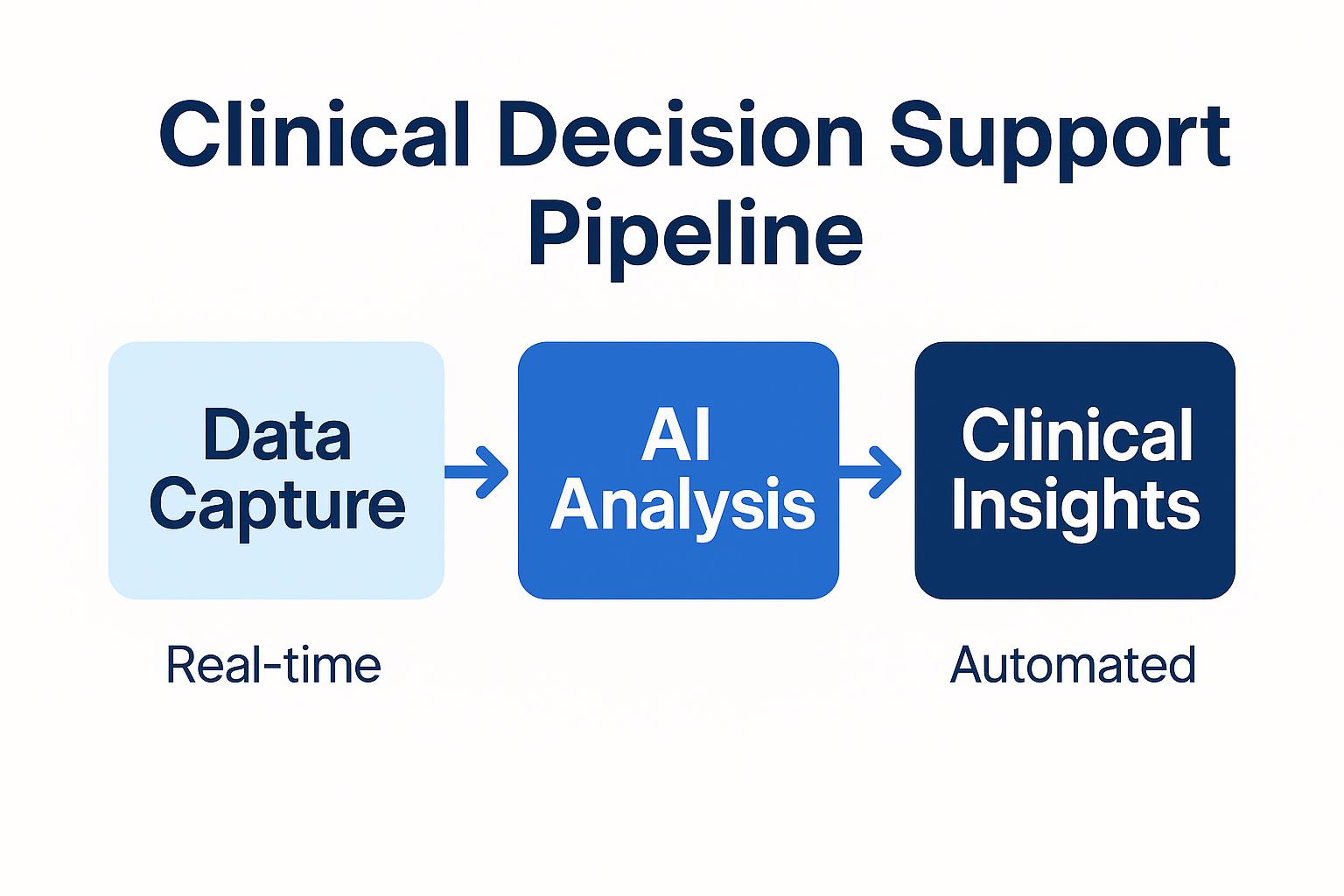
Real-time Data Integration and Decision Support
Continuous data capture and analysis allow clinicians to make timely, informed decisions based on comprehensive, current information. This real-time approach supports better patient outcomes and operational efficiency.
Enhanced Security and Compliance Monitoring
Automation platforms can detect unauthorized access, monitor data transfers for compliance violations, and generate detailed HIPAA and GDPR audit reports. These capabilities help organizations maintain regulatory compliance while enabling innovation.
What Are the Most Impactful Healthcare Workflow Automation Applications?
1. Intelligent Patient Engagement and Care Coordination
Omnichannel systems using text, email, mobile apps, and portals deliver personalized communications and integrate with care-coordination workflows. This trend makes healthcare mobile app development essential to modern care delivery. This growing reliance on technology has made healthcare mobile app development a critical component of modern care delivery.
2. Advanced Revenue Cycle Management
AI, ML, and RPA automate significant portions of the revenue cycle from registration to final payment, dramatically reducing denials and improving cash flow. Automated systems handle routine billing tasks while flagging complex cases for human review.
3. Clinical Decision Support and Documentation
AI-powered documentation tools capture visits and generate medical notes for clinician review, cutting administrative burden that can consume significant portions of a provider's day. These systems improve accuracy while reducing documentation time.
4. Automated Resource Management and Optimization
Predictive systems analyze patient volumes, demand patterns, and resource utilization to drive staffing and capacity decisions. Healthcare organizations can optimize their operations based on data-driven insights rather than historical patterns alone.
5. Laboratory and Diagnostic Workflow Integration
Automated lab systems validate results, identify inconsistencies, and route findings while maintaining full audit trails. Integration with other clinical systems ensures results reach the right providers at the right time.
6. Supply Chain and Inventory Management
Predictive analytics and real-time monitoring optimize inventory, trigger re-orders, and reduce waste. Healthcare organizations can maintain adequate supplies while minimizing carrying costs and expiration losses.
What Technologies Enable Advanced Healthcare Workflow Automation?
Artificial Intelligence and Machine Learning Integration
AI and ML analyze vast healthcare datasets, both structured and unstructured, to identify patterns, make predictions, and generate recommendations. These technologies enable more sophisticated automation than traditional rule-based systems.
Hyperautomation and Multi-Technology Integration
Hyperautomation combines AI, ML, and RPA to deliver end-to-end process optimization. This approach addresses complex workflows that require multiple types of automation working together.
Internet of Medical Things (IoMT) and Connected Devices
Connected devices stream real-time vitals, adherence data, and environmental metrics that AI systems analyze to predict risks and recommend interventions. This integration extends automation beyond traditional IT systems to include medical devices and monitoring equipment.
Cloud-Native Architecture and Scalability
Cloud platforms offer the elasticity and cost efficiency needed for real-time analytics and decision support at scale. Healthcare organizations can implement automation without significant upfront infrastructure investments.
Advanced Analytics and Business Intelligence
Real-time processing plus historical analysis provide actionable insights for administrators and continuous measurement of automation impact. These capabilities enable data-driven decision making across healthcare organizations.
What Is Real-time Adaptive Workflow Intelligence and Dynamic Optimization?
Predictive Analytics and Proactive Resource Management
Systems forecast admissions, identify ED bottlenecks, and optimize staffing and equipment maintenance. Healthcare organizations can anticipate needs rather than simply responding to current conditions.
Multi-Variable Optimization and Competing Objectives
Algorithms balance patient safety, efficiency, cost, and compliance while continuously recalibrating as conditions change. This holistic approach considers multiple factors simultaneously rather than optimizing single metrics.
How Can the Use of Data to Support Healthcare Organizational Workflow Excellence?
Real-time data integration from EHRs, devices, scheduling, and staffing systems fuels instant decision-making. Comprehensive monitoring enables healthcare organizations to respond quickly to changing conditions while maintaining quality standards.
The use of data to support healthcare organizational workflow optimization extends beyond simple metrics collection. Advanced analytics platforms process information from multiple sources to identify patterns and recommend improvements that enhance both efficiency and patient care quality.
Emergency Response and Crisis Management Capabilities
Adaptive platforms reconfigure workflows and resource allocation in seconds during surges, shortages, or equipment failures. These capabilities ensure continuity of care even under challenging circumstances.
What Are the Leading Healthcare Workflow Automation Platforms?
Comprehensive Healthcare Information Systems
Epic, Cerner, and Allscripts integrate clinical, administrative, and financial operations within unified architectures. These platforms provide broad functionality but may require significant customization for specific workflows.
Specialized Automation and Integration Platforms
Kareo for practice management and RCM, and DocuTap for urgent-care workflows deliver deep functionality for targeted use cases. These specialized solutions often integrate more easily with existing systems.
AI-Powered Clinical Decision Support Systems
Platforms analyze patient data and clinical guidelines to support diagnostics, treatment, and care coordination. These systems enhance clinical decision-making without replacing physician judgment.
Cloud-Native Integration and Data Management Solutions
Robust integration hubs unify data across diverse systems while enforcing security and compliance. These platforms enable comprehensive automation by connecting previously siloed systems.
How Do You Select Optimal Healthcare Automation Solutions?
Comprehensive Needs Assessment and Strategic Alignment
Map pain points to organizational goals and digital-transformation strategies. Understanding current challenges ensures automation investments address real problems rather than implementing technology for its own sake.
Integration Capabilities and Technical Architecture
Evaluate APIs, data formats, and workflow-integration requirements. Healthcare automation succeeds only when systems can exchange information seamlessly across the entire technology ecosystem.
Security, Compliance and Risk Management
Ensure HIPAA and GDPR compliance, encryption, role-based access control, and incident-response procedures. Healthcare automation must maintain the highest security standards while enabling operational improvements.
Scalability, Performance and Total Cost of Ownership
Assess growth capacity, maintenance needs, and long-term economics. Automation solutions should scale with organizational growth while maintaining cost-effectiveness over time.
User Experience and Change Management Support
Look for intuitive user interfaces and strong vendor training and resources. Successful automation requires user adoption, which depends on ease of use and adequate support during implementation.
How Does Modern Integration Support Healthcare Workflows?
Airbyte addresses healthcare data-integration challenges with 600+ pre-built connectors. Specialized support for HL7, FHIR, DICOM, and Change Data Capture keeps patient information synchronized in real time while meeting HIPAA standards.
Advanced Healthcare Data Integration Capabilities
Airbyte's Connector Development Kit lets teams build custom connectors for proprietary devices or applications with features designed to support security and compliance best practices. This flexibility enables integration with specialized healthcare systems that lack standard APIs.
Enabling AI-Powered Healthcare Workflows
Integration with vector databases and AI platforms provides the comprehensive data foundation required for predictive analytics, clinical decision support, and automated workflow optimization. Healthcare organizations can leverage their existing data investments to enable advanced automation capabilities.
Streamlining Healthcare Data Management
Modern integration platforms handle the complexity of healthcare data formats while maintaining audit trails and compliance requirements. This approach enables healthcare organizations to focus on patient care rather than data management challenges.
What Does the Future Hold for Healthcare Workflow Automation?
Emerging trends include autonomous healthcare agents capable of managing entire episodes of care and digital twin technology for simulating and optimizing operations before real-world deployment. Advanced interoperability standards leveraging blockchain for secure, seamless data exchange are also gaining traction.
Quantum computing may enable previously unattainable predictive-analytics performance, while natural language processing continues improving clinical documentation and patient communication. These technologies will further enhance the use of data to support healthcare organizational workflow optimization and patient care delivery.
Conclusion
Healthcare workflow automation represents a transformative opportunity for organizations to improve patient care while addressing operational challenges through intelligent use of data and technology. By implementing comprehensive automation strategies that integrate seamlessly with existing systems, healthcare organizations can enhance efficiency, reduce costs, and enable clinical teams to focus on high-value patient care activities. The key to success lies in selecting solutions that balance technological capability with practical implementation requirements while maintaining the security and compliance standards that healthcare demands.
Frequently Asked Questions
What Are the Most Critical Success Factors for Implementation?
Thorough workflow assessment, seamless integration, robust security and compliance measures, clear metrics, and strong change-management programs determine automation success. Organizations must engage stakeholders early and maintain focus on patient care outcomes throughout the implementation process.
How Do Organizations Measure ROI from Healthcare Automation?
Track labor savings, error reduction, revenue improvement, patient-outcome metrics, and qualitative measures such as staff and patient satisfaction. Successful measurement requires baseline establishment before implementation and ongoing monitoring of key performance indicators.
What Security and Compliance Considerations Are Essential?
Encryption in transit and at rest, role-based access control aligned with clinical workflows, comprehensive audit logs, and incident-response protocols that uphold HIPAA and GDPR requirements. Security must be built into automation solutions from the ground up rather than added as an afterthought.
How Can Organizations Avoid Common Pitfalls in Automation Projects?
Engage stakeholders early, prioritize change management, accurately scope integration complexity, and focus on patient-care outcomes rather than just technology implementation. Successful automation requires organizational commitment beyond technical deployment.
Which Emerging Technologies Will Have the Biggest Impact on Healthcare Workflows?
Generative AI for documentation, predictive analytics for proactive care, digital twins for operational optimization, and next-generation interoperability frameworks show the most promise for transforming healthcare workflows. These technologies will further enhance how organizations use data to support healthcare organizational workflow excellence.

.webp)
