Healthcare Data Integration: Benefits and Best Practices
Summarize this article with:
✨ AI Generated Summary
In the healthcare sector, data forms a crucial foundation of effective patient care, facilitating informed decision-making and improved outcomes. However, patient information is often dispersed across various systems, leading to fragmented health records that could result in misinterpretations or missed diagnoses.
Healthcare organizations worldwide are grappling with an unprecedented explosion of digital health information. The challenge lies not just in the volume of data being generated, but in the complexity of integrating diverse data sources while maintaining security, compliance, and real-time accessibility for clinical decision-making.
Therefore, to overcome this challenge, you must integrate data from disparate sources to create a holistic view of the patient's health profile. Research indicates that the global healthcare data integration market was USD 1.34 billion in 2023 and is anticipated to reach USD 4.51 billion by 2032.
In this article, you'll understand the significance of healthcare data integration, the potential challenges, and best practices to overcome them, along with emerging trends that are reshaping how healthcare organizations approach data integration.
TL;DR: Healthcare Data Integration at a Glance
- Healthcare data integration consolidates information from multiple sources like EHRs and wearable devices into unified datasets for comprehensive patient care
- Key use cases include patient-360 views, drug discovery acceleration, crisis response coordination, and population health management initiatives
- Major challenges involve standardization gaps, legacy system complexity, escalating security concerns, and regulatory compliance requirements
- Best practices emphasize FHIR standards adoption, scalable integration architectures, robust data quality frameworks, and comprehensive governance protocols
- Modern platforms like Airbyte streamline healthcare data integration through 600+ connectors and enterprise-grade security features
What Is Healthcare Data Integration and Why Does It Matter?
Healthcare data integration is the process of consolidating information from multiple sources, like electronic health records (EHRs) and wearable devices, into a single, cohesive dataset. By centralizing this data, you can gain a comprehensive view of a patient's medical history. This greatly simplifies workflows and empowers you to make timely decisions, leading to better patient care.
The importance of data integration in healthcare is underscored by the explosive growth of big data in the healthcare industry. According to market research, estimates for the big data in healthcare market size in 2024 generally range from USD 33 billion to USD 56 billion, with projections for 2032 varying widely from about USD 74 billion to over USD 180 billion, depending on the source.
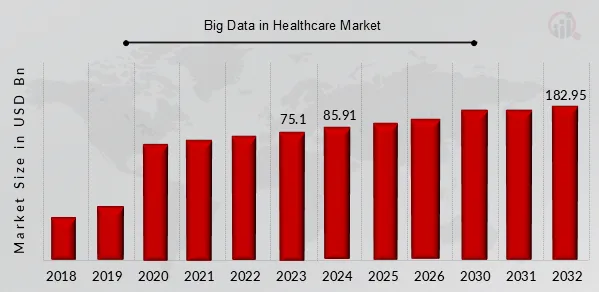
This surge highlights the increasing volume, variety, and velocity of data being generated from various sources. Big data integration helps you harness this wealth of information, enabling you to identify trends, improve operational efficiencies, and enhance clinical outcomes.
Modern healthcare data integration extends far beyond simple data consolidation. It encompasses the systematic process of combining disparate healthcare information sources into unified, actionable datasets that drive clinical decision-making and operational efficiency. The evolution from traditional paper-based systems to digital health ecosystems has created unprecedented opportunities for healthcare providers to leverage real-time data analytics, predictive modeling, and population health management initiatives that fundamentally reshape how care is delivered and coordinated across the healthcare continuum.
How Can You Successfully Integrate Healthcare Data?
Let's explore the various approaches you can use to perform healthcare data integration:
Data Streaming
Data streaming facilitates real-time integration of healthcare data, which is critical for applications like remote patient monitoring and emergency response systems. This approach allows for the immediate capture and analysis of patient data as it is generated, enhancing patient care by enabling timely interventions and improving overall responsiveness within healthcare systems.
Modern streaming architectures can process millions of data points from connected medical devices, wearable sensors, and continuous monitoring equipment while maintaining the low-latency requirements essential for critical care applications.
Application Integration
Application integration involves connecting disparate healthcare applications to facilitate data exchange and interoperability. This could be achieved through APIs, which allow diverse software systems to communicate effectively.
For instance, you can integrate EHR with a pharmacy management application to ensure that prescriptions are automatically updated and accessible across care teams. Modern application integration also encompasses the implementation of FHIR standards, which enable seamless data exchange between different vendor systems and support the development of innovative healthcare applications that can access patient data across multiple organizations.
Data Virtualization
Data virtualization lets you access and query data from multiple sources without physically moving it into a central repository. This approach creates a virtual data layer that enables you to integrate information on demand, providing real-time insights while reducing storage costs.
With data virtualization, you can create reports that combine information from EHRs, clinical trials, and public health databases without duplicating sensitive data. This approach is particularly valuable for healthcare organizations that need to maintain data sovereignty while enabling cross-institutional research and collaborative care initiatives.
What Are the Primary Use Cases for Healthcare Data Integration?
Patient-360 View
The patient-360 view refers to a unified view of patient data that enables you to gain a complete, holistic understanding of a patient. This data may include EHR records, medical history, insurance claims data, lab results, demographic data, and imaging systems. With this single source of truth, you can identify patterns in patient behavior, devise better diagnoses, and deliver personalized care.
Leading healthcare systems like Mayo Clinic have demonstrated the transformative impact of comprehensive patient-360 views through their unified EHR implementation across multiple campuses. Their system reduced duplication of tests while improving diagnostic accuracy and care coordination, enabling specialists across different locations to collaborate more effectively on complex patient cases.
The centralized data repository architecture facilitates quick retrieval of comprehensive patient histories, leading to increased diagnostic accuracy and improved clinical decision-making.
Drug Discovery
Developing a new drug is a complex process that requires extensive time, research, and financial resources. Healthcare data integration facilitates access to relevant information from different datasets, which can be used to advance research in drug development. Further, the integration of data from clinical trials and scientific publications provides a more holistic view of drug efficacy and safety.
Modern drug discovery initiatives are leveraging integrated genomics data, clinical outcomes, and real-world evidence to accelerate the identification of promising therapeutic targets. Healthcare data integration enables researchers to analyze encrypted patient information across multiple institutions without compromising individual privacy, supporting collaborative research efforts that can significantly reduce the time and cost associated with bringing new medications to market.
Crisis Response
Integrated healthcare data is vital for effective crisis response. During times of crisis, such as a pandemic or natural disaster, this data helps you make informed decisions, ensuring optimal care for patients and safety for frontline workers.
The COVID-19 pandemic demonstrated the critical importance of integrated healthcare data for effective public health response. Health information exchanges enabled real-time data sharing for disease surveillance, outbreak response, and resource allocation decisions.
Successful regional consortiums achieved significant improvements in emergency response capabilities by implementing standardized data sharing protocols that facilitated rapid identification of disease trends and coordinated response efforts across multiple healthcare organizations.
Population Health Management
Data integration lets you analyze big datasets to spot trends and patterns in certain groups of people. This information can then be used to identify risk factors and develop targeted interventions such as vaccination campaigns or chronic disease management programs, improving public health outcomes.
Advanced population health management programs are utilizing integrated data platforms to implement sophisticated analytics and reporting capabilities that support quality improvement and population health management activities. Organizations like Queen's Health Systems have successfully implemented custom algorithms to identify patients with undiagnosed conditions who were previously hidden within electronic medical record systems, enabling proactive outreach and care coordination to ensure appropriate preventive care services are delivered in a timely manner.
What Are the Key Challenges in Healthcare Data Integration?
Lack of Standardization
Healthcare data often comes from various sources, such as imaging systems and clinical notes, which can have different formats, codes, and terminologies. Lack of standardization can lead to inconsistencies and errors, making it difficult to analyze information effectively.
The challenge is compounded by the diversity of clinical terminology systems, where the same medical condition might be described using different terms and coding systems across various platforms. Laboratory data presents additional standardization challenges, with different systems potentially using varying units of measurement for the same tests.
These semantic differences make it extremely difficult to aggregate and analyze data across systems, even when technical connectivity exists.
Complexity of Legacy Systems
Many healthcare providers still rely on outdated legacy systems that are incompatible with modern technologies. These systems often require significant resources to integrate with new solutions, creating barriers to effective data sharing and increasing operational costs.
Legacy healthcare systems frequently use proprietary protocols or outdated standards that are incompatible with newer integration approaches, creating gaps in comprehensive data sharing initiatives. The coexistence of multiple protocol versions and proprietary communication methods creates an environment where successful data exchange requires careful coordination and often custom integration development.
Healthcare organizations with complex patchworks of legacy systems face unique vulnerability profiles, with numerous weak points in network infrastructure that may go unpatched or remain poorly managed due to resource constraints or operational priorities.
Data Security Concerns
Data security is a major concern in healthcare, especially as cyber threats continue to rise. In 2024, 67% of surveyed healthcare organizations experienced ransomware attacks. Protecting sensitive information is crucial for compliance and maintaining patient trust.
The expanding attack surface created by data integration initiatives poses significant security challenges for healthcare organizations. As systems become more interconnected and data flows increase across organizational boundaries, the number of potential entry points for malicious actors multiplies accordingly.
Healthcare organizations face unique vulnerability profiles compared to other industries, with interconnected medical devices, cloud platforms, and legacy systems creating numerous potential security weaknesses that must be carefully managed.
Data Quality Issues
Inaccurate or incomplete data can arise from inconsistent data entry practices or discrepancies between different systems. Relying on such data can lead to misinformed clinical decisions and hinder effective patient care.
Patient identification and matching represent fundamental challenges that undermine healthcare data integration efforts and can lead to serious safety and quality issues throughout the healthcare system. Variations in how patient demographic information is captured, stored, and maintained across different healthcare systems can create situations where the same patient appears as multiple distinct individuals in integrated databases, or conversely, where different patients are incorrectly merged into single records.
Regulatory and Compliance Complexities
The regulatory landscape surrounding healthcare data integration presents a complex web of requirements that organizations must navigate carefully to ensure compliance while enabling effective data sharing and interoperability. Multiple regulatory frameworks operate simultaneously, creating overlapping and sometimes conflicting requirements that must be reconciled in integration project planning and implementation.
HIPAA compliance in integrated environments requires careful attention to data flow mapping, access control implementation, and audit trail maintenance across multiple connected systems. The 21st Century Cures Act has introduced additional regulatory considerations focused specifically on interoperability and data sharing requirements, with enforcement mechanisms that include substantial financial penalties for organizations found to be engaging in information blocking practices.
What Are the Best Practices for Healthcare Data Integration?
1. Identify and Document Data Sources
Start by identifying all potential data sources across your healthcare ecosystem—EHRs, laboratory test results, insurance systems, patient portals—and document where critical data resides, how it flows, and any dependencies involved.
Comprehensive data source mapping should extend beyond traditional clinical systems to encompass emerging data sources such as wearable devices, patient-generated health data, and social determinants of health information. This mapping process should also document data ownership, stewardship responsibilities, and existing integration points to identify opportunities for consolidation and optimization.
2. Design Scalable Integration Solutions
As your organization expands, scalability becomes essential. Choose integration solutions that can adapt to new systems and data sources while handling increasing volumes without compromising performance.
Modern scalable integration architectures should incorporate cloud-native designs and microservices-based approaches that can accommodate exponential data growth while maintaining performance and reliability standards. The integration platform should support both real-time streaming data and traditional batch processing to address diverse healthcare use cases while providing the flexibility to evolve with changing organizational needs.
3. Implement Industry Standards
Use standardized frameworks like Fast Healthcare Interoperability Resources (FHIR) to exchange data among diverse healthcare systems, enhancing interoperability.
FHIR adoption has accelerated dramatically, with nearly 90% of health systems implementing FHIR-enabled APIs. The standard's RESTful API architecture makes it significantly easier for developers to build applications that can interact with multiple healthcare systems without requiring custom integration work for each platform.
Organizations should also consider implementing emerging standards like openEHR for vendor-neutral data foundations that support long-term strategic goals.
4. Ensure Data Quality
Implement data validation and cleansing processes. Regularly assess accuracy, completeness, and consistency, and leverage healthcare workflow automation to reduce errors.
Advanced data quality management should incorporate machine learning algorithms that can identify patterns in data quality issues and automatically correct common problems. AI systems can detect duplicate records, identify inconsistent data formats, and flag potential data entry errors that might otherwise go unnoticed until they impact clinical or operational processes.
5. Enhance Data Security Protocols
Enforce encryption, multi-factor authentication, and regular security audits to safeguard patient data and ensure compliance with regulations such as HIPAA.
Modern security approaches should incorporate Zero Trust architectures that operate on the principle of "never trust, always verify," requiring continuous authentication and authorization for every access request regardless of the user's location or network connection. Healthcare organizations should implement comprehensive security controls that can manage thousands of connected devices while providing network segmentation and micro-perimeters that isolate critical systems.
6. Establish Data Governance
Implement a comprehensive data governance framework covering data availability, usability, integrity, and security. Define ownership, access rights, and stewardship responsibilities.
Effective data governance frameworks must address the secondary use of healthcare data for research, quality improvement, and population health management activities while ensuring appropriate privacy protection and compliance with research ethics requirements. Clear policies and procedures for data de-identification, research data use agreements, and institutional review board oversight ensure that healthcare data integration supports valuable research activities while maintaining patient privacy and regulatory compliance.
How Are Real-Time Data Processing and Advanced Integration Architectures Transforming Healthcare?
Real-time data processing and advanced integration architectures are revolutionizing healthcare data integration by enabling immediate access to critical patient information and supporting time-sensitive clinical decision-making. Healthcare environments generate continuous streams of data from patient monitoring devices, electronic health records, laboratory systems, and connected medical equipment, creating both opportunities and challenges for organizations seeking to leverage this information for improved patient outcomes.
Edge Computing and Point-of-Care Integration
Edge computing technologies are transforming healthcare data integration by enabling real-time processing of critical patient information at the point of care. Rather than relying on centralized cloud infrastructure that may introduce latency or connectivity issues, edge computing systems process data locally using computing resources deployed near medical devices and clinical areas.
This approach is particularly valuable for time-sensitive applications such as patient monitoring, where delays in data processing could impact patient safety. The integration of edge computing with Internet of Things medical devices is creating new possibilities for continuous patient monitoring and automated clinical decision support.
Wearable cardiac monitors can now analyze heart rhythm data locally and trigger immediate alerts when dangerous arrhythmias are detected, without waiting for data to be transmitted to remote servers and processed. Smart infusion pumps incorporate advanced safety features and connectivity to clinical systems, helping reduce medication errors and support treatment precision. However, fully autonomous adjustment of medication dosages based on continuous vital sign measurements from patient monitoring devices is not yet a widespread feature.
Hospital operations are being transformed by edge computing systems that can coordinate multiple IoT devices and clinical systems in real-time. Operating rooms equipped with edge computing capabilities can provide surgeons with real-time analytics during procedures, enhancing surgical precision and patient outcomes.
The deployment of edge computing in healthcare environments requires careful consideration of security and integration challenges, as edge devices must be secured against cyber threats while maintaining the performance and reliability necessary for critical healthcare applications.
Streaming Data Architectures and Event-Driven Processing
Real-time data streaming architectures are being integrated with edge computing systems to create comprehensive data processing pipelines that span from medical devices to enterprise analytics platforms. These architectures enable healthcare organizations to process time-sensitive data at the edge while also feeding information into larger data integration systems for long-term analysis and reporting.
The combination of edge processing and streaming data architectures is enabling new applications such as predictive maintenance for medical equipment and automated quality monitoring for clinical processes. Event-driven processing models are becoming increasingly important for healthcare organizations that need to respond immediately to changing patient conditions or system alerts.
These architectures can process millions of data points from connected medical devices and continuous monitoring equipment while maintaining the low-latency requirements essential for critical care applications. The implementation of real-time capabilities requires sophisticated infrastructure investments and technical expertise, but organizations report significant benefits in terms of improved patient safety and clinical outcomes.
Advanced Data Architecture Paradigms
Data mesh and data fabric architectures represent a fundamental shift in how healthcare organizations approach data integration and management. These decentralized approaches recognize that traditional centralized data warehouses and lakes are insufficient for the scale and complexity of modern healthcare data ecosystems.
Data mesh architectures treat data as a product, with domain-specific teams taking ownership of their respective data assets while ensuring these assets remain discoverable and accessible to other parts of the organization. In healthcare applications, data mesh architectures enable clinical departments to maintain control over their specialized data while contributing to enterprise-wide analytics capabilities.
Cardiology departments can manage their imaging and diagnostic data as a specialized product while ensuring this information integrates seamlessly with patient records maintained by other departments. This approach reduces the bottlenecks associated with centralized IT teams managing all data integration efforts while ensuring that domain experts who best understand the data context maintain responsibility for data quality and governance.
Data fabric architectures complement data mesh approaches by providing the underlying infrastructure necessary to support decentralized data management. These architectures create a unified layer of abstraction across hybrid and multi-cloud environments, enabling seamless data access regardless of where information is physically stored.
Healthcare organizations can integrate data from on-premises electronic health record systems with cloud-based analytics platforms and external data sources such as public health databases or research repositories while maintaining consistent security and governance controls across all environments.
How Can Airbyte Streamline Healthcare Data Integration?
Manually consolidating data from multiple healthcare sources can be error-prone and time-consuming. To automate this process, you can leverage Airbyte, a robust data integration and replication tool that supports more than 600+ pre-built connectors.
Key Features of Airbyte for Healthcare Organizations
- Flexible Pipeline Development – Build pipelines via an intuitive UI, powerful APIs, a Terraform provider, or PyAirbyte to support diverse healthcare IT environments and integration requirements.
- Custom Connectors – Use the Connector Builder or CDK—complete with AI-assist—to create connectors when one doesn't yet exist, enabling integration with specialized healthcare systems and legacy applications.
- GenAI Workflows – Load unstructured data into vector stores (Pinecone, Chroma, Weaviate) for AI-driven similarity searches, supporting advanced healthcare analytics and clinical decision support applications.
- Change Data Capture – Detect changes in the source dataset and replicate them downstream to maintain consistency, ensuring real-time synchronization of critical patient information across healthcare systems.
- Data Pipeline Orchestration – Integrate with Dagster, Apache Airflow, Prefect, and Kestra to support complex healthcare data workflows and existing enterprise orchestration platforms.
- Automatic Detection of Dropped Records – Monitor record counts across source, platform, and destination layers, alerting you to discrepancies that could impact patient safety or regulatory compliance.
- Schema Change Management – Automatically detect and propagate schema changes from source to destination, supporting the dynamic nature of healthcare data systems and evolving clinical requirements.
- Self-Managed Enterprise – The Enterprise edition supports multi-tenancy, RBAC, PII masking, and more, providing the governance and security controls essential for healthcare organizations.
- Enhanced Security – Features include encryption, authentication, access controls, and audit logging, with compliance to HIPAA, GDPR, SOC 2, and ISO 27001, ensuring healthcare organizations can meet the most stringent regulatory requirements.
Airbyte's open-source foundation eliminates vendor lock-in concerns that often prevent healthcare organizations from adopting new data integration platforms, while the enterprise features provide the security and governance capabilities required for sensitive patient data. The platform's support for both cloud and on-premises deployments enables healthcare organizations to maintain data sovereignty requirements while accessing modern integration capabilities that support advanced analytics and interoperability initiatives.
Wrapping Up
This article highlighted the critical role of healthcare data integration in providing high-quality patient care and operational efficiency. You've explored key use cases—patient-360 views, drug discovery, crisis response, and population health management—as well as major challenges including data standardization, legacy system complexity, and security concerns.
The emergence of advanced technologies like AI, edge computing, and digital twins is transforming how healthcare organizations approach data integration, creating new opportunities for improved patient outcomes and innovative care delivery models.
By following these guidelines and leveraging modern integration platforms like Airbyte, healthcare organizations can create more efficient, secure, and patient-focused systems that support both current operational needs and future innovation requirements.
Frequently Asked Questions
1. What is the difference between ETL and ELT in healthcare data integration?
ETL (Extract, Transform, Load) transforms healthcare data before loading, ensuring strict standardization and compliance—ideal for regulated environments like EHR integration. ELT loads raw data first, enabling scalable, on-demand transformations for analytics and AI-driven insights in modern cloud healthcare platforms.
2. How does FHIR improve healthcare data interoperability?
FHIR (Fast Healthcare Interoperability Resources) provides a modern, RESTful API-based standard that enables seamless data exchange between different healthcare systems. It simplifies integration development, supports mobile and web applications, and has been widely adopted across healthcare organizations, with nearly 90% of health systems implementing FHIR-enabled APIs.
3. What are the main security challenges in healthcare data integration?
Healthcare data integration faces unique security challenges including the expanded attack surface from interconnected systems, the need to protect sensitive patient information across multiple platforms, compliance with regulations like HIPAA and GDPR, and managing security for thousands of connected medical devices while maintaining system performance and availability.
4. How can healthcare organizations ensure data quality in integrated systems?
Organizations should implement comprehensive data validation and cleansing processes, use machine learning algorithms to identify and correct data quality issues automatically, establish robust data governance frameworks, and implement patient matching technologies to prevent duplicate records and ensure accurate patient identification across systems.
5. What role does artificial intelligence play in healthcare data integration?
AI technologies automate data normalization processes, improve data quality through pattern recognition and error detection, enable natural language processing of unstructured clinical data, support federated learning for collaborative research, and provide predictive analytics capabilities that enhance clinical decision-making and population health management.

.webp)
.png)