CTO's Guide to Healthcare Data Sovereignty: HIPAA-Compliant Hybrid Deployment
Summarize this article with:
✨ AI Generated Summary
Healthcare organizations face a critical challenge balancing HIPAA-compliant data sovereignty with the need for agile, real-time analytics. Hybrid architectures separate cloud-managed control planes from on-premises data planes, ensuring protected health information (PHI) remains within approved jurisdictions while leveraging cloud orchestration for scalability and performance.
- Hybrid models keep PHI on-premises or in private clouds, moving only metadata to the cloud, reducing compliance risks and audit complexity.
- They provide high availability, lower infrastructure overhead, and seamless interoperability with healthcare standards and 600+ connectors.
- Key design steps include scoped data planes, encrypted channels, regional control planes, and immutable audit trails to meet HIPAA and data residency laws.
- This approach enables faster deployment, improved clinical performance, and secure, compliant AI-ready data pipelines without sacrificing control or security.
You're expected to deliver real-time clinical insights while HIPAA, HITRUST, and a patchwork of regional data-residency laws cover every record you move. An infrastructure that misses a single safeguard can put your hospital on the wrong side of a federal investigation.
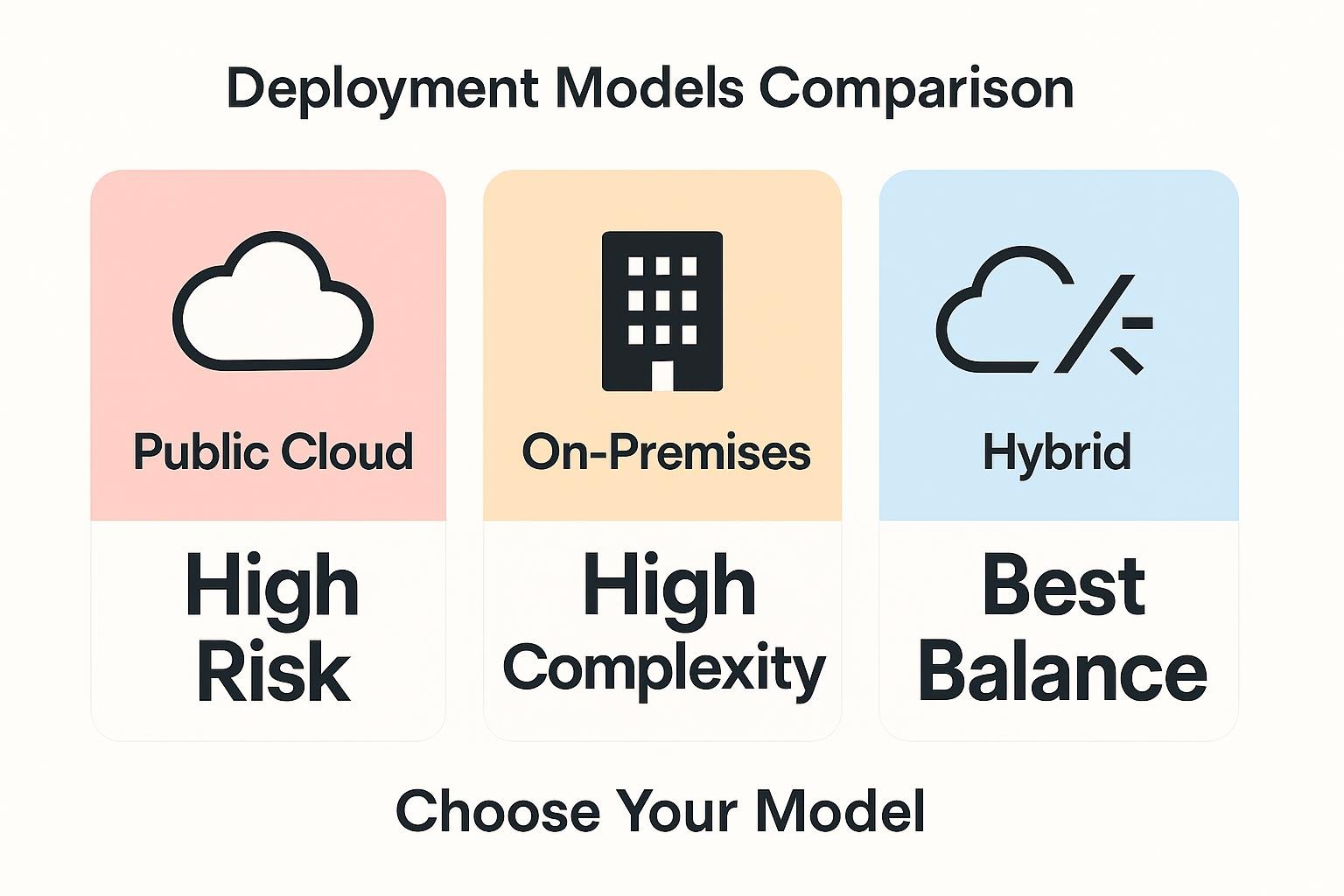
Pure public cloud often stores control-plane metadata outside approved jurisdictions, risking unauthorized exposure of protected health information. Keeping everything on-prem solves sovereignty but slows the analytics your clinicians need and forces your team into endless hardware and Kubernetes maintenance. Compliance or agility feels like a coin toss you can't win.
Hybrid deployment rewrites that trade-off. By splitting a cloud control plane from hospital-controlled data planes, you keep PHI inside your network while still scaling analytics in minutes.
What Does Data Sovereignty Mean for Healthcare CTOs?
Data sovereignty means you, not a cloud vendor, decide where protected health information (PHI) lives, who can access it, and how it moves. Under the HIPAA Security Rule, every replica, log, and backup of electronic PHI must remain protected according to strict safeguards, even if managed by third-party service providers under a Business Associate Agreement. Multinational providers must also respect GDPR's strict border controls on patient data.
When data moves outside these boundaries, you assume breach liability even if the violation happens inside a vendor's platform. That's why many healthcare CTOs avoid cloud-based data platforms entirely.
From a technical perspective, sovereignty comes down to three control points:
- Physical location of storage
- Identity authentication for each request
- Pathways that process or replicate data
Multi-tenant SaaS ingestion, off-region backups, or control-plane metadata that lands in foreign data centers all break that chain of custody.
Zero-trust practices (strong MFA, least-privilege roles, outbound-only network traffic) close many gaps, but only if you control where workloads run and logs are stored. Hybrid architectures solve this by splitting a cloud control plane from an on-prem or private-VPC data plane. PHI stays inside hospital walls while cloud-based orchestration handles scheduling and monitoring.
The following table illustrates how different deployment models balance these critical factors:
Why Traditional Cloud Models Fail Healthcare Compliance?
Public clouds weren't designed for regulated workloads. Their global control planes log credentials, metrics, and job metadata on infrastructure you don't own, often in regions you can't name. Once that metadata leaves your jurisdiction, you lose the demonstrable "custody" HIPAA demands.
Pushing raw clinical data into SaaS pipelines amplifies this problem. Each hop through an unmanaged service violates HIPAA's minimum-necessary rule and creates new breach vectors you can't audit. Common incidents include:
- Hospitals syncing EHR extracts through U.S. vendors while treating EU patients
- Monitoring agents streaming PHI-laden logs to overseas regions
- Multi-tenant analytics platforms exposing shared storage buckets across customers
The financial consequences are severe. OCR fines can reach up to $50,000 per violation (with annual caps), and settlements routinely exceed millions when investigators discover uncontrolled cloud transfers of protected health information. Reputational fallout compounds the damage as regulators broadcast violations, eroding trust with clinicians and patients alike.
This reality demands an architecture that preserves performance without surrendering data control.
How Hybrid Deployments Enable HIPAA-Compliant Data Sovereignty?
A hybrid architecture splits responsibility between a cloud-managed control plane and one or more local data planes. You keep PHI inside hospital-controlled infrastructure while letting the cloud schedule jobs, surface logs, and expose APIs. The control plane never touches raw data, avoiding the compliance gap that arises when public clouds replicate or back up information across regions.
PHI is extracted, transformed, and loaded entirely within a private VPC or on-prem cluster. Only lightweight metadata (pipeline IDs, job status, connector versions) travels to the control plane through outbound-only traffic, so you don't need to open inbound firewall ports. This arrangement satisfies HIPAA's technical safeguards by maintaining custody of sensitive records while providing cloud orchestration elasticity.
Here's how the hybrid model distributes responsibilities:
This separation preserves data sovereignty without sacrificing cloud-level convenience.
Airbyte Enterprise Flex exemplifies this pattern. You run the identical 600+ connectors inside your environment, but scheduling and monitoring happen in Airbyte's cloud (no feature trade-offs, no vendor lock-in, and no PHI crossing jurisdictional lines). The product launched specifically to address data sovereignty mandates in regulated industries and AI workloads that need regional separation of training data.
What Are the Core Benefits of a HIPAA-Compliant Hybrid Model?
A hybrid control-plane architecture gives healthcare teams cloud agility while keeping protected health information (PHI) under their control. Key benefits include:
- Guaranteed Data Sovereignty: PHI stays on-premises or in your private cloud, while only metadata moves through the control plane. This setup meets HIPAA and data residency requirements and makes audit tracing simple.
- Reduced Audit and Breach Risk: Immutable local logs and external secrets management ensure full visibility and Zero Trust protection, allowing fast proof of data custody and limited exposure to compromised accounts.
- High Availability and Performance: Regional data planes keep latency low for clinical systems and support cloud bursting for analytics, providing both speed and scalability.
- Lower Infrastructure Overhead: Cloud-managed orchestration, updates, and monitoring remove manual maintenance. You pay only for active compute. This drives down total cost compared with legacy ETL middleware and self-managed integration stacks.
- Seamless Interoperability Across Systems: A unified hybrid setup supports 600+ connectors and common healthcare standards (HL7 FHIR, OMOP CDM, HL7 v2), ensuring consistent data exchange across EHRs, LIMS, imaging, and billing systems.
Together, these advantages help healthcare organizations maintain compliance, improve care delivery, and modernize operations without sacrificing control or security.
How CTOs Should Design a Hybrid Healthcare Data Architecture?
Before you spin up Kubernetes clusters or sign a new cloud contract, map the decisions that keep protected health information (PHI) under your control. Your hybrid architecture needs to balance local custody with cloud capabilities. These five steps provide a framework that satisfies HIPAA while staying responsive to clinical demands.
1. Identify Regulated Data Classes
Trace every PHI touchpoint in your environment, from EHR tables to imaging archives. Label each dataset by sensitivity and jurisdiction. This inventory lets you separate low-risk analytics feeds from high-risk records that must stay on-premises. You'll satisfy HIPAA's data minimization rule and support ongoing audits with clear data boundaries.
2. Deploy Scoped Data Planes
Place workloads that handle PHI inside hospital-controlled hardware, a HITRUST-certified private cloud, or an edge cluster at the care site. Processing close to the bedside cuts latency and avoids cross-border transfers. Size these planes for peak clinical load and let bursty analytics run elsewhere.
3. Use External Secrets and Encrypted Channels
Route all credentials through an enterprise key vault instead of storing database passwords in application pods. Enforce TLS 1.2+ for every hop. Continuous key rotation and least-privilege roles shrink the blast radius of any breach.
4. Configure Regional Control Planes
Use cloud orchestration for scheduling and observability, but ensure it exchanges only metadata (never raw PHI) with your data planes. Multi-region support keeps distributed hospitals under one management interface without violating residency laws.
5. Implement Immutable Audit Trails
Stream detailed logs (from query traces to schema changes) into an on-premises SIEM. Immutable storage meets HIPAA's six-year retention rule and accelerates incident forensics. With end-to-end evidence in place, you can prove compliance before auditors ask.
What Results Can Healthcare CTOs Expect?
Healthcare teams report significantly lower infrastructure costs when moving from legacy ETL to hybrid control-plane architectures. Deployment cycles compress from months to weeks using pre-built connectors and cloud-managed orchestration.
Local data planes with regional failover deliver high uptime for critical systems. Bed-occupancy dashboards and lab-result alerts maintain availability during provider outages. PHI processing stays within your network perimeter, transforming HIPAA audit preparation from reactive compliance exercises to systematic log reviews.
Clinical teams gain sub-minute dashboard updates, streamlined research cohort assembly, and operational analytics without regulatory violations. This performance improvement directly translates to better patient outcomes and more efficient care delivery workflows.
Why Hybrid Is the Future of Healthcare Data Infrastructure?
Hybrid architectures enable local PHI custody with cloud-scale analytics, addressing the fundamental tension between compliance requirements and operational agility. As regulatory scrutiny intensifies around data sovereignty, control planes in the cloud with on-premises data planes have become essential for maintaining compliance while delivering modern capabilities.
Evolving healthcare demands around AI and precision medicine require elastic resources without sacrificing data sovereignty. Airbyte Enterprise Flex delivers the same 600+ connectors with hybrid control plane architecture that keeps your data under your control, representing the next generation of healthcare data infrastructure that balances innovation with protection.
The future belongs to organizations that can move fast without moving their data. Talk to our sales team to see how Airbyte Enterprise Flex delivers a HIPAA-compliant hybrid architecture that keeps ePHI in your VPC while enabling AI-ready clinical data pipelines.
Frequently Asked Questions
What is the difference between a control plane and a data plane in hybrid architectures?
The control plane manages orchestration, scheduling, and monitoring in the cloud without touching your actual data. The data plane runs inside your infrastructure (on-prem or private VPC) and processes all PHI. This separation lets you maintain complete data sovereignty while using cloud convenience for management tasks.
How does a hybrid deployment satisfy HIPAA's technical safeguards?
A hybrid deployment keeps all PHI within your controlled environment where you maintain encryption, access controls, and audit logs. Only non-sensitive metadata (job status, pipeline IDs) travels to the cloud control plane through outbound-only connections. This approach meets HIPAA requirements for administrative, physical, and technical safeguards without exposing protected health information to unauthorized access.
Can I use the same connectors across cloud and on-premises deployments?
Yes. Airbyte Flex provides the same 600+ connectors across all deployment models. You run identical code whether processing data on-premises, in a private VPC, or in the cloud. This consistency eliminates the feature trade-offs that plague other hybrid solutions and lets you reuse pipelines as your infrastructure evolves.
What happens to my audit logs in a hybrid architecture?
Your audit logs stay inside your network perimeter when using a properly designed hybrid deployment. Every pipeline run, schema change, and access request writes to immutable logs you control. You can stream these logs to your on-premises SIEM for centralized monitoring while maintaining the six-year retention HIPAA requires. The cloud control plane never stores PHI-laden logs.

.webp)